Introduction
Before open-heart surgery, doctors don’t rely on guesswork. They use proven tools to estimate risk - one of the most important is the STS risk score. But how is this number calculated?
This guide explains the inputs and process behind the STS calculator, helping patients understand why doctors use it and what it means for surgical planning.
The Basics of the STS Calculator
The Society of Thoracic Surgeons (STS) risk calculator is a web-based tool built on decades of real world surgical data. By entering patient-specific information, it predicts the chance of:
- Death after surgery
- Major complications (stroke, kidney failure, prolonged ventilation, infection)
- Length of hospital stay
It’s updated regularly to reflect the latest outcomes from across the U.S., making it one of the most accurate medical calculators in use.
Key Patient Factors in the Score
The STS calculator considers dozens of factors. Some of the most important include:
- Age: Older patients generally carry higher risk.
- Sex: Men and women may have slightly different risk profiles.
- Heart function: Measured by the ejection fraction (EF), which shows how well the heart pumps blood.
- Kidney function: Lab tests like creatinine levels influence risk.
- Lung function: Conditions like COPD can increase complications.
- Diabetes: Especially if insulin-dependent.
- Other health issues: Stroke history, vascular disease, liver disease.
- Urgency of surgery: Emergency procedures carry higher risk than scheduled ones.
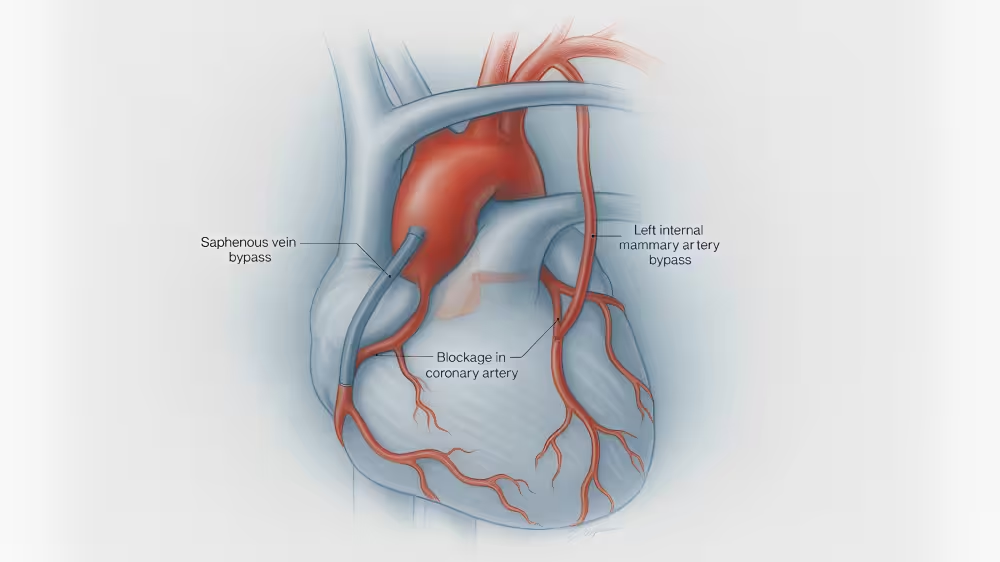
- Procedure type: CABG, valve replacement, or combined surgery each carry different risk levels.
These inputs are entered into the calculator and weighted according to how strongly they predict outcomes.
What the Score Produces
The output of the STS calculator is **a set of percentages**. For example, it might show:
- 1.5% chance of death
- 3.2% chance of stroke
- 5.0% chance of kidney failure
- 6.7% chance of prolonged ventilation
Together, these numbers give a clearer picture of the overall risk profile for surgery.

Why It Matters for Patients
For patients, the calculation has real value:
- Transparency: It shows how your individual health affects your risk.
- Decision-making: Helps compare surgery against less invasive treatments.
- Hospital planning: High-risk patients may need specialized care settings.
- Recovery planning: Anticipating possible complications can help families prepare.
It ensures that patients and doctors are speaking from the same evidence-based foundation.
Limitations of the Calculation
Even the best calculators have limits. The STS score cannot:
- Predict the exact outcome for one person
- Capture unique factors like emotional strength or family support
- Account for every new technology or surgical innovation
That’s why it’s always combined with surgeon judgment - numbers alone never make the final decision.
Key Takeaways
- The STS risk score is built from dozens of health and procedure factors.
- It predicts percentages for death and complications after surgery.
- It guides planning but is not the sole deciding factor.
---
If you'd like to better understand how your STS score was calculated and what it means for your surgery, Verus can help. We combine AI-powered analysis with surgeon expertise to explain your risk clearly and personally.