Pain Management After Heart Surgery: Your First 6 Weeks at Home
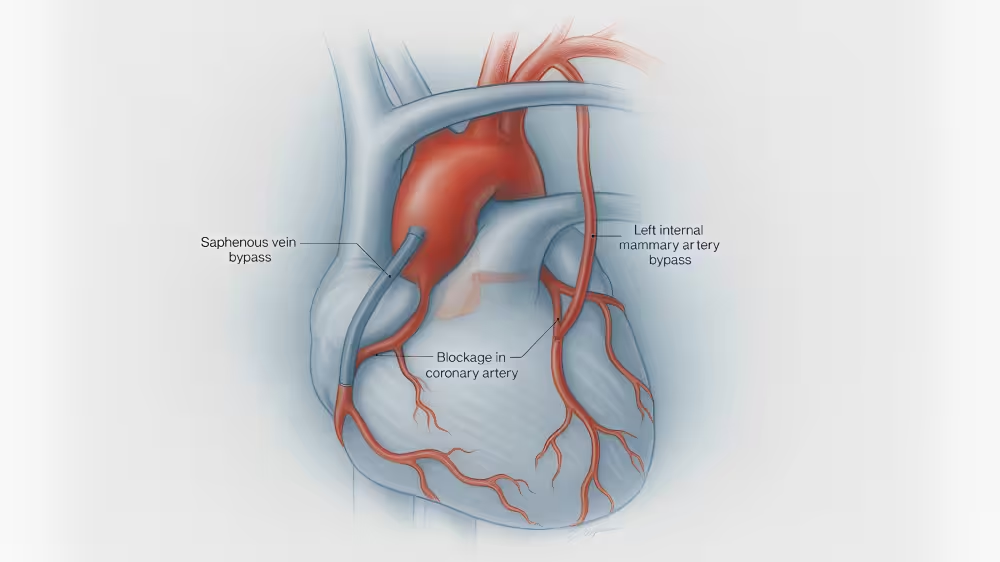
Maria, 68, went home three days after her bypass. The first week, getting out of bed and coughing hurt the most. By week three, she still felt sore, but walks were longer and sleep came easier. Maria’s story is typical: recovery isn’t painless, but with a plan - medications plus simple daily habits - most patients feel steady improvement week by week.
What follows is a practical, step-by-step guide for patients and families across the U.S. Always follow your surgical team’s instructions; plans vary by hospital and by patient.
What Pain Is “Normal” vs. Concerning (Weeks 1–6)
Common / expected:
- Achy, sore, tight feeling in the chest and shoulders, worse with movement or deep breathing
- Incision tenderness (chest and any leg/arm vein harvest sites)
- Brief “zingers” or tingling as nerves wake up
- Back / neck stiffness from surgery positioning and sleep adjustments
Less common - call your team:
- Pain that is rapidly worsening or not improving week to week
- New, sharp pain at rest, especially with shortness of breath, dizziness, or sweating
- Marked swelling, heat, or drainage at any incision
Emergency - call 911:
- Crushing chest pain, severe shortness of breath, fainting, or signs of stroke (face droop, arm weakness, speech difficulty)
Medications: A Deeper Dive (Scheduling, Typical Duration, Taper Concepts)
Goals:
- Keep a steady “base” of comfort.
- Use short-acting medicine only for breakthrough pain.
- Stop or taper medicines as pain improves.
Typical components after discharge (examples; your regimen may differ):
- Acetaminophen (base layer): Often scheduled around the clock for the first 1–2 weeks, then as needed. Helps reduce the need for stronger meds. Avoid doubling up with combo products.
- Anti-inflammatories (NSAIDs): Some programs use them briefly; others avoid due to kidney/bleeding concerns. Only use if your surgical team says it’s okay.
- Nerve-calming medicine (e.g., gabapentin/pregabalin): Sometimes used for nerve-type pain or sleep disruption. Usually short term (days to a few weeks) and then tapered off.
- Topicals: Lidocaine patches or similar can help chest-wall or shoulder soreness. Do not place directly on an incision unless your team approves.
- Opioid (short course, for breakthrough pain): Intended for the first few days to a week, then tapered off as activity increases.
- Bowel regimen while on opioids: Stool softener ± gentle laxative; hydrate and walk to keep things moving.
How to schedule your day (example pattern):
- Morning: base medicine; consider a topical; short walk after
- Midday: base medicine; ice or heat (not on incisions) for 15–20 minutes
- Late afternoon / Evening: base medicine; another short walk; gentle stretches
- Bedtime: if evenings are your worst time, take your scheduled base dose; use pillows to support a comfortable position
Opioid taper concept (example—confirm specifics with your team):
- Use the smallest amount needed for movement-related pain in days 1–3.
- When pain eases, reduce by one tablet per day every day or two.
- Switch remaining doses to bedtime only if sleep is the last hurdle.
- Stop when you’re comfortable on the base layer and non-drug strategies.
Safety: Lock medications away, never share, and do not drive while taking opioids.
Non-Drug Strategies: A Simple DailyChecklist
Every morning
- Breathing: 5-10 slow breaths with your incentive spirometer; splint with a pillow to support your chest
- Walk #1: Start with short, flat walks; add a little distance daily.
- Pain plan: Take your base medicine on schedule; track your pain score (0–10).
Midday
- Walk #2: Repeat; gentle pace.
- Comfort: Ice or heat to shoulders/back (not over incisions).
- Fuel: Hydrate; include protein at meals to support healing.
Afternoon / Evening
- Walk #3 (and #4 if able): Short and steady wins.
- Stretch: Gentle shoulder rolls and ankle pumps; no pushing or pulling through the arms.
- Wind-down: Dim lights, limit screens, and set up pillows before bed.
Bedtime
- Position: Back-sleeping with pillows under knees, or side-sleeping with a pillow hugging your chest if your team allows and you are comfortable.
- Sleep routine: Aim for consistent bed/wake times.
Every day
- Incision check: Redness, spreading warmth, opening, thick drainage? Call your team.
- Bowels: If no bowel movement by day 2–3 at home, contact your team for guidance.
- Progress log: Note steps walked, pain triggers that improved, and what helped.
Incision-SpecificGuidance
A) Sternal (chest) pain focus
- Splinting: Hug a small pillow when coughing, sneezing, or standing up.
- Movements: Use the “log-roll” to get out of bed; keep your shoulders moving gently but avoid pushing/pulling heavy loads.
- Lifting: Keep things light (think: lighter than a gallon of milk) until your team clears you.
- Cough and breathe: Don’t skip breathing exercises—preventing pneumonia actually reduces pain over time.
- Driving: Wait for your surgeon’s clearance and never drive while taking opioids.
B) Leg/arm vein-harvest site tips
- Elevation: Prop the limb so the incision is above heart level several times a day to reduce swelling.
- Compression: Wear stockings if prescribed; remove as directed for bathing and skin checks.
- Motion: Gentle ankle pumps and short walks improve circulation and comfort.
- Skin care: Keep clean and dry; avoid soaking (baths, pools) until cleared; moisturize surrounding skin - not the incision - if dry or itchy.
Sleep, Mood, AndEnergy
- It’s common to feel more sore in the evening. Plan your walks earlier and arrange pillows before fatigue sets in.
- Short naps are okay; long daytime sleep can worsen night sleep.
- Low mood or irritability is common early on and often improves as pain eases. Tell your team if sadness, anxiety, or poor sleep persist.
When To Call Vs. Go To The ER
Call your surgical team within 24 hours if you notice:
- Fever, chills, or flu-like feelings
- Increasing redness, warmth, or drainage at any incision
- New swelling in one calf or significant swelling at a harvest site
- Pain that is not improving week to week or is limiting walking and deep breathing
Call 911 now for:
- Crushing chest pain, severe shortness of breath, fainting, or sudden neurologic symptoms (facedroop, arm weakness, speech trouble).
Frequently Asked Questions
How long will pain last?
- Most patients feel meaningful improvement every week; many are much better by weeks 4–6.
Will I become dependent on pain pills?
- Short-term, planned use with a taper is the safest approach. If you’re worried, tell your team early - they can adjust the plan.
Can I use a heating pad over my chest incision?
- Not directly on the incision. Use heat or ice around the shoulders/back only, with a cloth layer to protect skin.
---
If you'd like a personalized recovery game plan or a clinician-ready summary to share at follow-up, explore the MyVerus Report and our services, or reach out directly. We’re here for you and your family.