Introduction
A heart transplant is one of the most complex and transformative surgeries in medicine. For patients with advanced heart failure, it may be the only option for survival and a return to meaningful quality of life. Yet the process - from evaluation to recovery - can feel overwhelming. This guide explains what to expect before, during, and after a heart transplant, with a focus on supporting patients and families through the journey.
Who Needs a Heart Transplant?
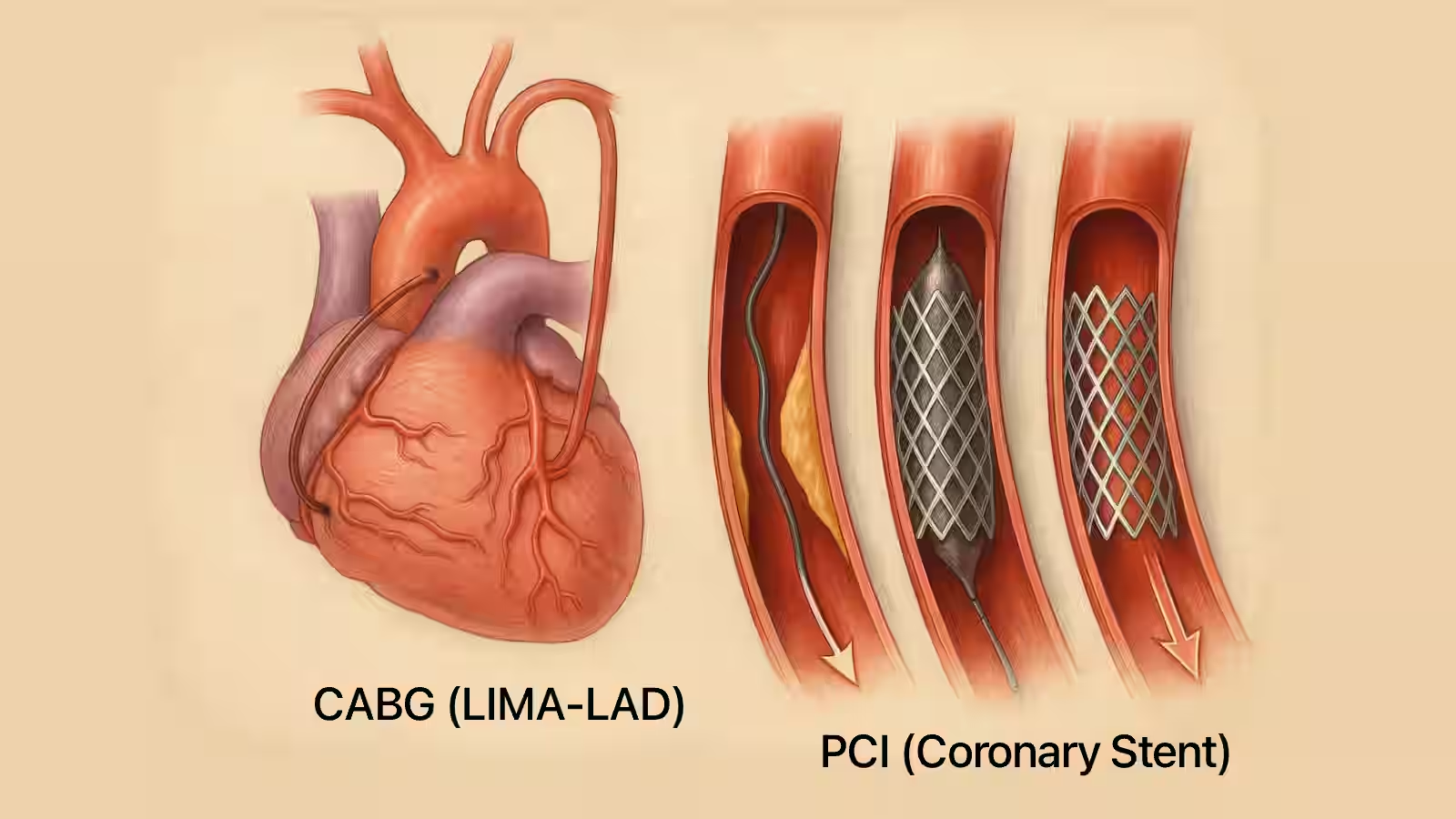
Not everyone with heart disease needs a transplant. Typically, candidates are patients with:
- Severe heart failure not responding to medication or devices
- Repeated hospitalizations for worsening heart function
- Life-threatening arrhythmias not controlled with therapy
- Inability to perform daily activities due to heart weakness
Doctors perform extensive testing to ensure patients are strong enough to undergo the surgery and recover afterward.
The Transplant Process
Evaluation: A team of specialists assesses heart function, other organ health, mental readiness, and family support.
Waiting List: Because donor hearts are scarce, patients are placed on a national waiting list. Urgency, blood type, size, and geography all play a role in matching.
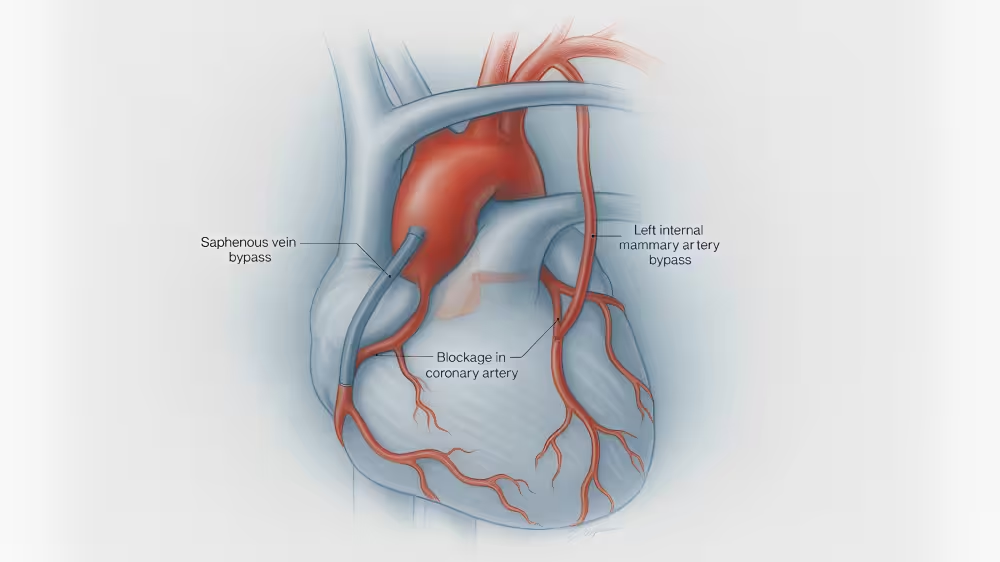
Surgery: Once a heart becomes available, surgery typically lasts 4–6 hours. The failing heart is removed, and the donor heart is sewn into place and connected to major blood vessels.
Life After Heart Transplant
Recovery doesn’t end when surgery is over. Patients and families must prepare for lifelong follow-up.
Hospital Recovery: Most patients spend 1-2 weeks in the hospital. Early physical therapy helps regain strength.
Immunosuppression: Because the immune system sees the donor heart as “foreign,” lifelong medications are needed to prevent rejection. These can increase infection risk, so regular monitoring is essential.
Rejection Surveillance: Routine heart biopsies, blood tests, and imaging help detect early signs of rejection or complications.
Lifestyle Changes: Healthy eating, regular exercise, avoiding tobacco and alcohol, and adhering to medications all support long-term success.
Risks and Challenges
Even with excellent care, risks remain. These include:
- Organ rejection
- Infections from immune suppression
- Kidney damage from medications
- Increased risk of certain cancers
- Emotional stress and anxiety for patients and families
The good news: with modern advances, average survival after heart transplant exceeds 12-15 years, and many patients live much longer.
Emotional and Family Support
A transplant affects the whole family. Common concerns include:
- Fear of rejection or complications
- Financial strain
- Emotional stress of caregiving
- Adjusting to a “new normal”
Support groups, counseling, and cardiac rehabilitation programs can make a meaningful difference.
Conclusion
A heart transplant is not just a surgery - it is a second chance at life. With preparation, family support, and close partnership with the care team, patients can look forward to many meaningful years ahead.
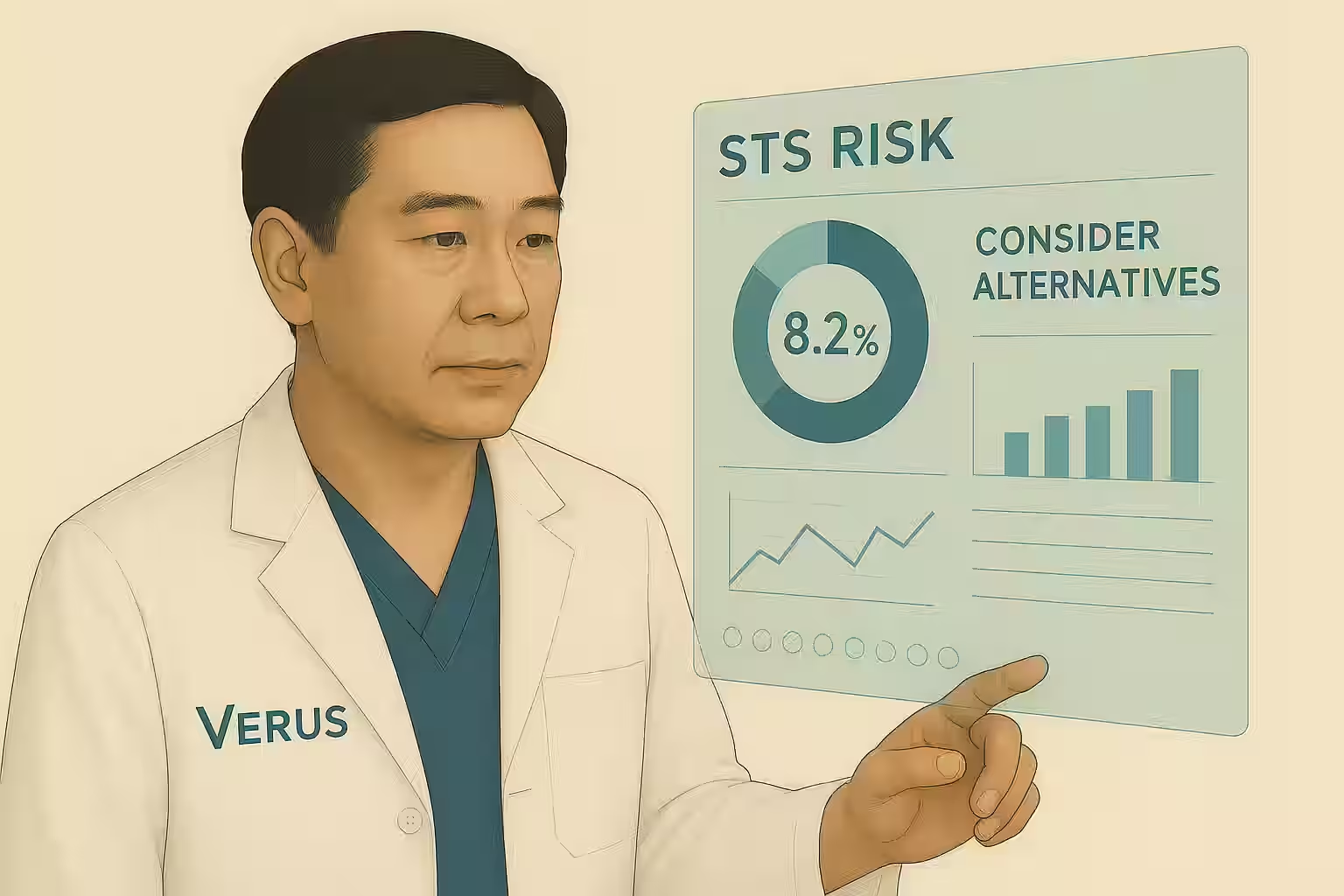
If you or a loved one are considering a transplant, the best first step is to seek a thorough evaluation and learn about your options. At Verus, we provide patients and families with clear, data-driven insights to guide decisions.