Introduction
Tricuspid regurgitation (TR) occurs when the tricuspid valve fails to close properly, allowing blood to flow backward from the right ventricle into the right atrium. Although often overlooked, severe TR can lead to right-sided heart failure, liver congestion, and fluid retention. Understanding when surgical repair versus replacement is optimal empowers patients and families to make informed decisions.
Understanding Tricuspid Regurgitation
Etiology and Classification
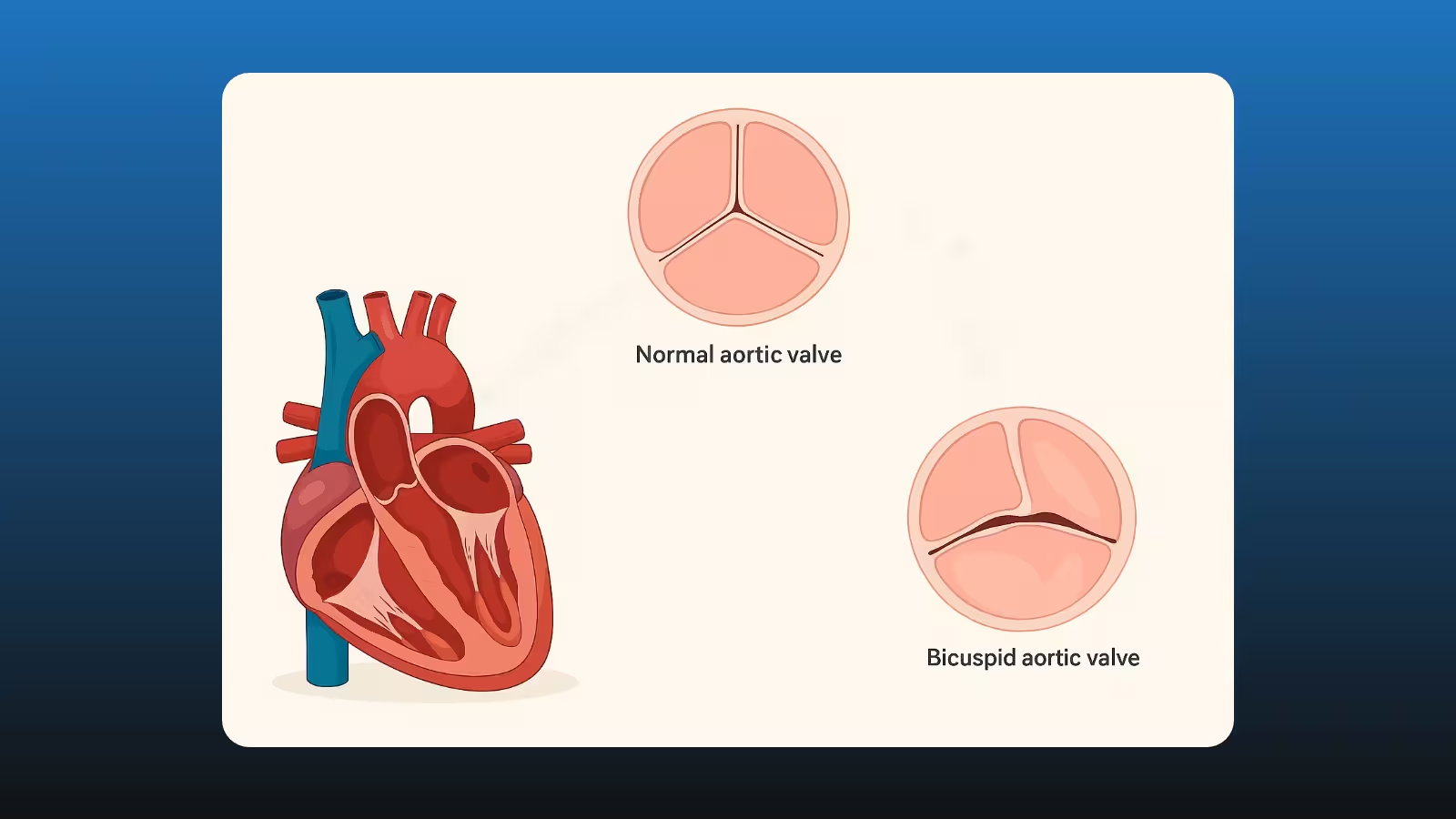
TR may be primary (structural valve disease) or secondary (dilation of the right ventricle / annulus). Common causes include:
- Secondary TR due to left-sided heart disease or pulmonary hypertension
- Primary TR from endocarditis, rheumatic disease, or congenital abnormalities
Severity is graded by echocardiography as mild, moderate, or severe based on regurgitant volume and vena contracta width.
Clinical Presentation
Symptoms often develop insidiously and include:
- Fatigue and weakness
- Abdominal bloating and swelling
- Jugular venous distension
- Hepatomegaly and ascites
When to Repair the Tricuspid Valve
Indications for Repair
Repair is preferred when the valve leaflets and subvalvular apparatus are intact, and annular dilation is the primary issue. Consider repair in:
- Severe functional TR at time of left-sided surgery
- Moderate TR with annular diameter ≥40 mm
- Symptomatic patients without advanced right ventricular dysfunction
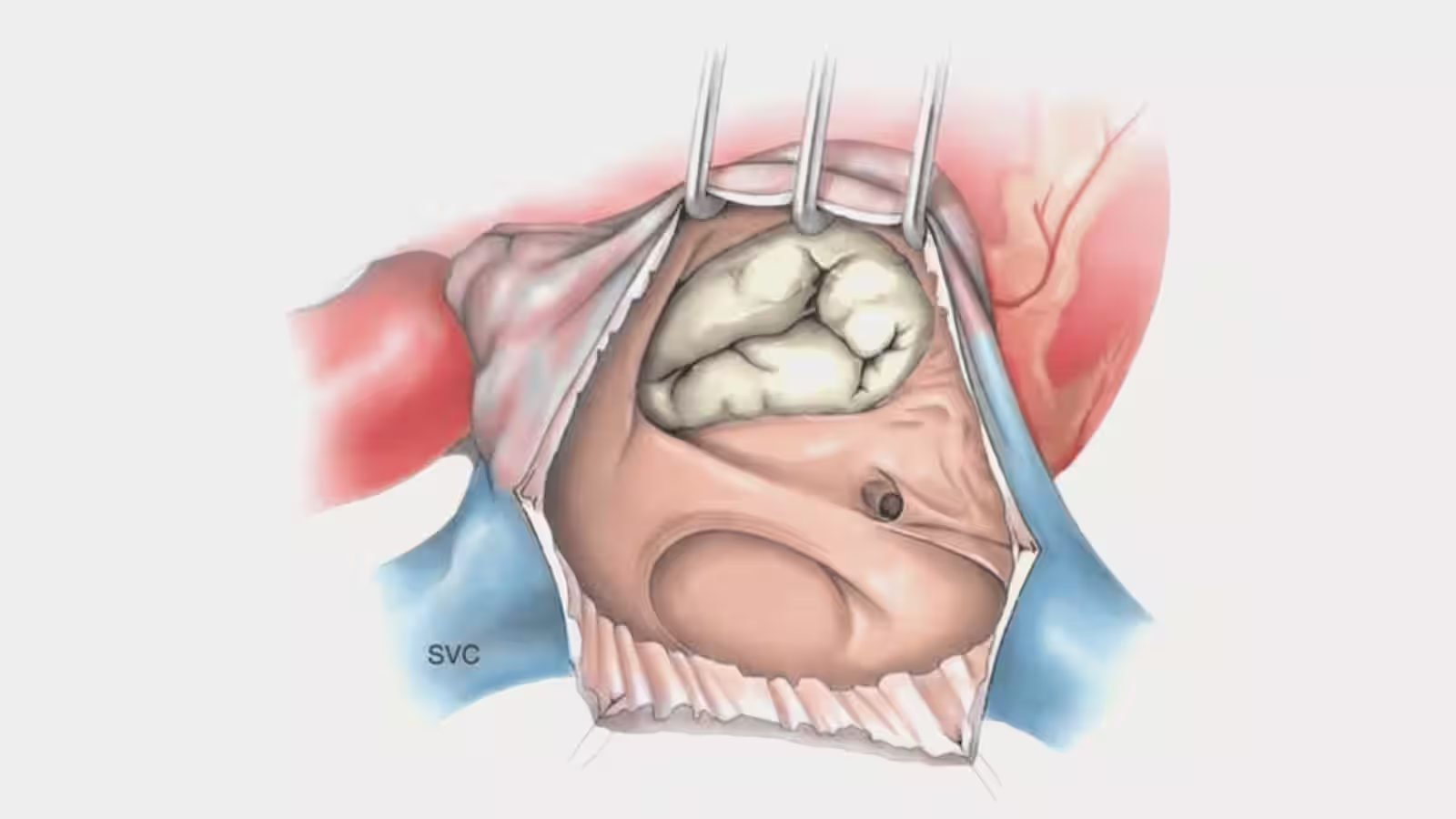
Repair Techniques
- Annuloplasty ring implantation to restore annular geometry
- Leaflet plication or edge-to-edge repair for localized leaflet prolapse
When Replacement Is Necessary
Indications for Replacement
Valve replacement is indicated when:
- Primary leaflet pathology (e.g., endocarditis, carcinoid)
- Repair failure or severe tethering of leaflets
- Recurrent TR after prior repair
Prosthetic Valve Options
- Bioprosthetic valves offer low thrombosis risk but limited durability
- Mechanical valves provide longevity but require lifelong anticoagulation
Peri-Operative and Post-Operative Considerations
Sternal Precautions
- Avoid lifting >10 lbs for 6-8 weeks
- Support chest when coughing or sneezing
Driving and Flying
- Resume driving after 4-6 weeks, once sternal stability is confirmed
- Flying is safe after sternal healing and stable anticoagulation
Plating vs. Wiring
- Sternal plating may improve comfort in high-risk patients
- Standard wiring remains effective for most cases
Recovery Timeline
Conclusion
Timely decision-making between tricuspid repair and replacement can preserve right ventricular function and improve quality of life. Patients and families are encouraged to discuss individual risk factors and surgical options with their cardiac surgeon.
---
Ready to explore your second opinion options? Book your complimentary call to get personalized guidance today.